The Regenerative Outcomes Foundation is proud to present the Pioneers of Hope, a series of our founder Doug Oliver’s personal interviews with leading influencers in the Regenerative Medicine movement. These articles are our way of sharing the hope that this field promises to all, from top legislators, great policy minds, researchers, patients, and providers, as well as many others around the world who are molding tomorrow’s discoveries with today’s visions.
Pioneers of Hope will inspire, impassion, and reveal the sentiment, experiences, and motivations that drive these special individuals with unique perspectives reminding us of our common humanity and shared goals for making regenerative health a reality.
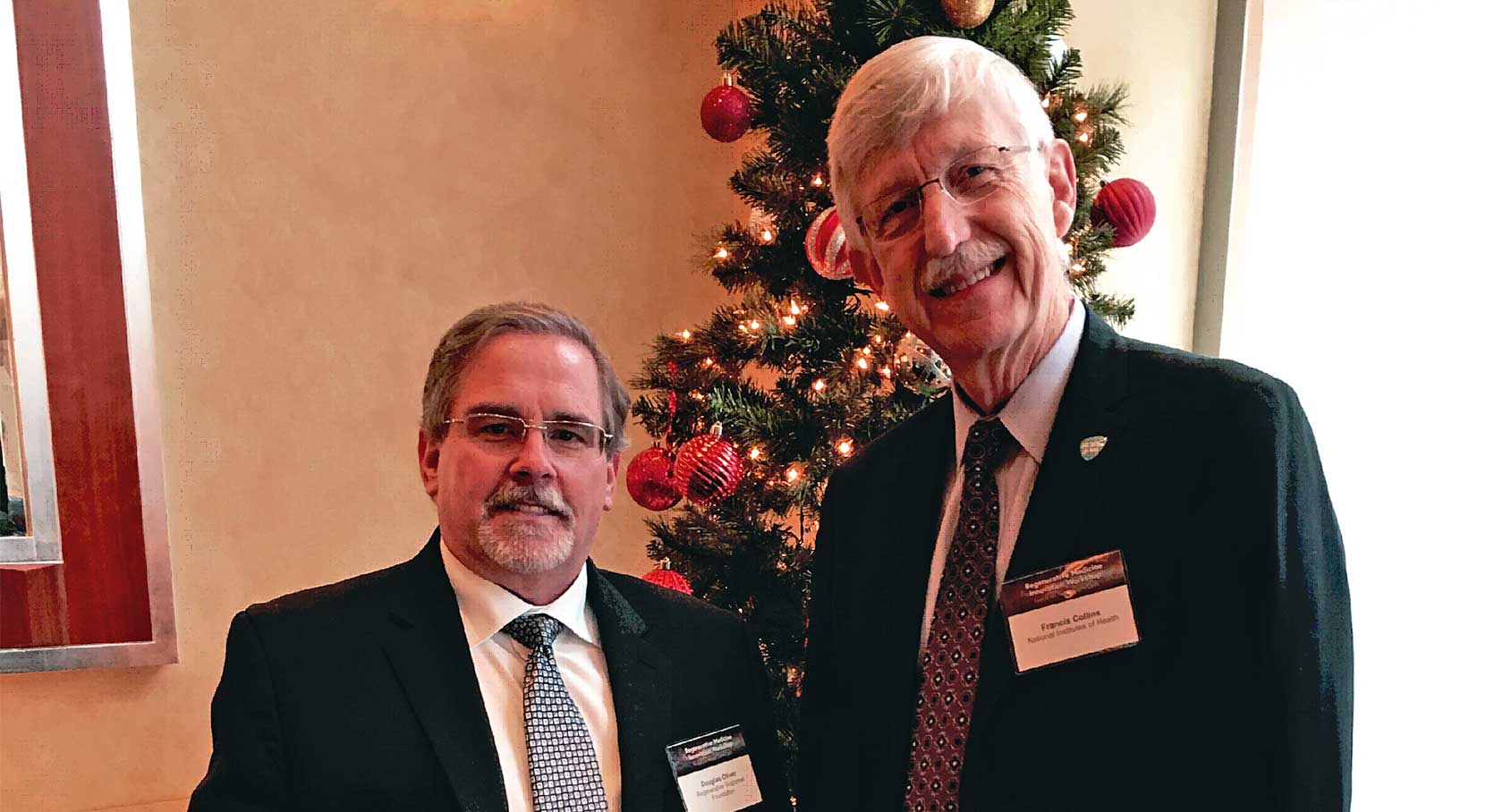
In support of our friends at The World Stem Cell Summit, we’re honored to offer this conversation with our first Pioneer of Hope, Dr. Francis Collins, Director of the National Institutes of Health.
Doug: Dr. Collins, thank you so much. This is a certainly a journey.
Francis: For all of us.
Doug: A friend and colleague on our board, Sammy Jo Wilkinson, and I were discussing our stories, tomorrow’s hearing, and our advocacy efforts for patient access to cell therapies. One year since Cures was passed, this has all now come full circle with the Bipartisan Policy Center and Senator Alexander, the Regrow Act, and even just yesterday the coalition the Foundation is now helping to build for approaching regulators in order to create a clinical cell therapy registry.
You and I are here with hundreds of others to celebrate the one year anniversary of the 21st Century Cures Act’s passage. Last week it was the anniversary of passage in the House, tomorrow it’s the Senate. I’ll be there enjoying your testimony. When the Cures bill was made law, Senator Alexander characterized the passage as a “Christmas Miracle.” Today, we’re standing in front of the Christmas tree at this conference one year later, and everything has been catalyzed with promise for patients. Everybody is excited. Truly, the possibilities for patients are exciting, but I’m reminded this season that so many are still suffering chronic and debilitating diseases. Nonetheless, we’re entering a time where hope is real and justified, like you have recently mentioned about Sickle Cell – a treatment… perhaps a cure… in five years. That’s real hope that we patients can hang onto, without a pat on the head and without the frustration of waiting and having that hope deferred unreasonably.
Francis: There’s a quote I’m very fond of about hope which comes to mind right now. Peter Levi, the British poet, said, “Hope in every sphere of life is a privilege that attaches to action. No action, no hope.” I get very frustrated when I hear people saying, “Well, I hope for this, or, it would be a hope of mine that…” Okay, let’s talk about what that means. What’s the privilege that you have now taken upon you, and how that means it has to be attached to an action plan.
Doug: I agree with you. On behalf of many, many patients we applaud you! As Director of the National Institutes of Health, how else can you remind us to continue cultivating our hope, especially within those of us who might be unable to engage you through formal systems? This is very important because the vast majority of patients in this new population are chronically debilitated. They have a limited voice by virtue of the energy it takes just to stay well. Know what I mean?
Francis: I do.
Doug: Given that, how do you interact with and engage patients at an informal level?
Francis: Well, we’re doing some of that right now. Certainly for me, as a physician who got interested in research as a means to try to find answers for those thousands of diseases for which we don’t have good solutions – the only way we’re really going to get there is to listen to the people who we’re trying to reach out to, and be sure we understand what, in fact, they’re looking for as far as outcomes. That era of participants in clinical research being called “human subjects” should be over. I hate that term, although it’s now somehow irreversibly put into regulatory language. Subjects? No. These are our partners. Everything, if I have a chance to be involved in it, about a clinical trial has those partners fully engaged. If they’re not able to be at the table physically because of limitations, we have other ways – with the amazing abilities available now through social networks – of reaching out to find out what they’re thinking. I can tell you about a particular effort I’m involved in right now to try to build a really effective research program on chronic fatigue syndrome. You talk about people who are in a very difficult place, many of them unable to even get out of bed, where research is critically necessarily to try to get some answers to this incredibly mysterious, puzzling, frustrating, awful disease. In the space of the last two years, we’ve gone from having very little effort in that space, to now, just funded a month or so ago, a whole bunch of centers of excellence to work on chronic fatigue syndrome.
Doug: Amazing.
Francis: We were very much informed by the information we were able to gather from those folks, many of them writing us e-mails from their bed, which is the best they were able to do. We’ve learned a lot from that.
Doug: Do you have ways of quantifying that are dependable, or is there an intuitive sense to it, maybe by committee choice or consensus internally?
Francis: Yeah. It’s more qualitative than quantitative, but it’s a lot better than where we were before. That input just wasn’t being heard. Now it needs to be heard in every way.
Doug: Do you see methods like this translating into regenerative medicine in other ways, not just with patients but those they are in relationship with? I’m thinking MS, muscular dystrophy, neurological conditions where it’s really the family that needs a lot of the voice. All of those diseases create significant limitations, requiring amazing adaptive skills, yet are nearly always very isolating for all involved. It’s about visibility as much as it is about voice.
Francis: It’s also about listening to those who you are hoping to help, about what they would see as the kind of outcomes that would matter. Clinicians sometimes have this idea, “A successful trial will be if we achieve the following endpoint,” and the people with a disorder are like, “I don’t care about that endpoint.”
Doug: “I want to be able to walk to my car.”
Francis: Exactly. So we have a program called Promise, which is a now-ten-year effort to actually, for a wide variety of medical conditions, find out from participants and trials, what are they looking for? Patient reported outcomes…
Doug: That is incredibly important. Is there a baseline measurement effort before the trial to establish the post-trial effect of that intervention? Because that’s a prime example of a behavioral intervention.
Francis: Yes. There absolutely is. Again, I would not want to see us now mounting trials for chronic illnesses that don’t include those inputs, as far as deciding “What is the outcome that we are actually going to judge whether the trial worked or not?” on.
Doug: What about intervening and introducing, through Cures, research of behavioral services in a co-study, to measure their impact? Comparing outcomes with behavioral services as opposed to outcomes where they are not offered. Is that something that’s a good idea?
Francis: Sure. I’ll jump into another thing that’s occupying a lot of my time right now, including a hearing yesterday, which is opioid addiction.
Doug: Mental health is a huge component there.
Francis: Absolutely huge. It’s one thing to say we have medication-assisted treatment, and we can now show that that is the way to help people get free of addiction. But wait a minute, there’s more than that going on.
Doug: That’s right.
Francis: So again, we have to listen to what our people’s actual hopes for getting free of addiction are. What does their life look like? Are we actually doing the right thing by just saying, “Well, your urine is clean now.”
Doug: Right. It’s an opportunity to develop new tools and get validation with different outcomes and different endpoints.
Francis: …To do this holistically. We’re really thinking about the whole person.
Doug: Thank you. Let’s move on to your thoughts on patient stakeholder status and self-determination. Part of the magic of the Cures Act is the idea that patients are now given status as bona fide stakeholders. I write about this, I talk about patients “getting up from the children’s table.”
Francis: That’s a good metaphor.
Doug: There’s a sequestering that has become part of the culture of regulatory practice, and part of what I’m trying to do as an ambassador – rather than a fist-in-the-air advocate – is to raise people’s awareness that that’s not good.
Francis: Yeah.
Doug: That’s not the purpose of Cures. I helped write part of the patient provisions, and it’s very clear that the legislators want real stakeholder status for patients, because we’re paying a lot of the bill now too. Health policy in the future is going to go in that direction, and everybody knows it. Given that we’re financial stakeholders, we’re believers, it’s essential that we remain up from the children’s table.
We’re also growing in knowledge, and patients accessing knowledge develops the one tool that’s most necessary for sustaining hope and autonomy: the hope that patients generate themselves by exercising self-determination. I know that there’s a balancing act happening out there when it comes to self-determination. One recent example would be the “right-to-try” laws coming into view. What is your view on self-determination and your experience with it? You’re a top observer, and one that sees both sides of this issue.
Francis: I think that’s a critical responsibility and opportunity for individuals who are seeking ways to help themselves through clinical research. I should point out that one of the other programs the Cures Act put substantial funding into is precision medicine, and this has led now to this All Of Us Program, which is going to enroll one million Americans over the course of the next two or three years in a long term study of health and illness – a broad spectrum of individuals across ages, geographies, race, ethnicity, socio-economic status – the largest such study that’s ever been mounted. But what is unique about it is that this is “participants at the table” in every way. Just what you’re talking about in terms of having the chance to be self-determined. If you’re in that program and you say, “I want to see my whole genome sequence” because you’ve had it determined, we’ll give it to you. None of this, “Oh, it might be bad for you. You might not understand it.” This is changing that dynamic pretty dramatically, and very much supporting the idea that people ought to be in charge of what happens to them in a clinical trial.
That’s going be an incredible platform. I mean, think about that. A million people. How many people there will have age-related macular degeneration? A lot. If you want to then mount a clinical trial of regenerative medicine for that, or for diabetes, arthritis, or anything that’s reasonably common, you’re going to have a pre-consented group of highly informed, motivated participants who are going to raise their hand and say, “Okay, talk to me about it.”
Doug: “Take my genome.”
Francis: Right. “Yeah, talk to me about your trial.” And you’ll already have this baseline of information that they’ve made available, including their electronic health records.
Doug: I recently had my own genome taken by NEI a few months ago. I know exactly what you’re talking about.
Francis: It’s empowering.
Doug: Nobody knows what’s going on with my eyes, not truly. I do have a clinical diagnosis, but it may not even be accurate. It has to be better understood, in order to have a chance of determining why the treatment I had worked for me.
This reminds me of a conversation I remember having in your office, you pointing your finger at me, and you said, “Doug, you’re in the 2%. I want to know why this worked for you.” I remember remarking, “You want to put money into little old me to figure it out?” and you said, “Absolutely, I’m going to find a way because…”
Francis: …even if you were N equals one, I’d want to know what happened.
Doug: That leads me to our next question. What is it that creates the spark for you to keep on doing such a hard job? Tell us a story or something that inspired you. Why do you keep on keeping on?
Francis: Oh, because it’s a joy to be part of something that has this kind of promise. This is not hypothetical, that we’re going to actually save lives and treat terrible illnesses. It’s happening, all the way back to when I was a faculty member at the University of Michigan and had the chance to discover the gene for cystic fibrosis. I dreamed how that would someday lead to treatments that are going to prolong the lives of these kids with this disease. Now that’s happening and you can see it. It’s not a dream of 100 years from now. I also work on one of the rarest diseases that affects kids with premature aging, something called progeria.
Doug: Wow.
Francis: In my own research lab, I discovered the cause, and within four years got to a clinical trial. I’m about to publish a paper showing its prolonged survival, substantially, and there’s a second clinical trial that I want to start sometime in the next year that I think will be even better. To be part of that, to be able to spend your time on something that has that kind of ability to change lives – that’s not hard at all. I mean, there are some things about being in charge of the largest biomedical research organization in the world, with a $36 billion budget, that does lead to a fair amount of complexity, but I’m not complaining. It’s a great opportunity.
Doug: So with progeria, it’s a single mutation, that’s easy to identify?
Francis: Yes.
Doug: So with these conditions, you’re actually making progress in a very interesting way. You’re understanding one mutation at a time, and then creating a hypothesis to move forward, is that right?
Francis: Exactly. Macular degeneration is probably a collection of a lot of other rare diseases.
Doug: I was at the House Oversight Committee Hearing last week, and will be at the Senate HELP Committee Oversight Hearing tomorrow. I saw you last week, and will see you again tomorrow?
Francis: Yes you will. You may get a shout out from Senator Alexander.
Doug: That would be great! We’re in full fundraising mode for the Foundation right now, so I’ll take it! We want to help patients with their expenses, travel, all of that. At the hearing last week, I noticed the interactions between you and Scott Gottlieb, Commissioner of the FDA, who was also testifying on his agency’s progress for 21st Century Cures. You and Dr. Gottlieb were chuckling and smiling – the camaraderie was palpable.
Francis: We get along really well.
Doug: That’s so refreshing for patients.
Francis: Yeah. That’s important.
Doug: You’re forming a good collaboration. Are you feeling positive about moving forward with that relationship?
Francis: Yeah. Look at today, which is very much constructed jointly between NIH and FDA. Peter Marx has been fantastic as a partner in putting this together. That was one of my goals when I first became NIH Director. It was to try to get NIH and FDA closer together. Also NIH and CDC.
Doug: But it takes two players.
Francis: It does.
Doug: What’s inspiring is your skill in actually making that happen. I think that might be historic. We are so gratified at the effort the two of you are making moving forward, and it appears to be successful.
Francis: You’ve got to put some time and effort into it. It doesn’t just happen with a phone call. You’ve got to build, not just at the top, but at levels all the way through.
Doug: Which you have now done with NIH, with each agency having an FDA liaison shoulder to shoulder with you. NIH agencies now meet separately and together using that model, and that’s wonderful. I’m deeply inspired.
Dr. Collins, as always, I appreciate the trust you’ve extended to our relationship, and I promise to maintain that trust. Thank you for being willing to see me in both vulnerable and excited frames of mind. We communicate fairly often on a number of different topics. Sometimes I’ve written you with sad stories, and other times I’ve written you with positive news. I am honored that despite that, you remain gracious toward me, offer wisdom, and still welcome me back.
My own journey has produced experiences that still have questions we all need answers to. It’s taught me the importance of faith. At this stage in regenerative medicine, we still know so little about not just the physical influences on patient outcomes, but the familial, social, spiritual, and financial disruptions some of these outcomes produce. They’re very real, and we need to understand them.
Francis: Yes.
Doug: I’m deeply inspired when I remember that you are a person of faith. I’m a person of faith. I’ve read your book, The Language of God. As we draw our time to a close, can we consider the season for a moment? It’s so meaningful to enter this time and space where we reflect on what has been done, what has been given, what has been prayed for, what has been achieved, and what’s been unsuccessful. Give us a personal glimpse of you, your guitar and piano playing, authoring, reflecting, and celebrating in the context of your faith – if you would give us that gift.
Francis: For me, faith is an anchor, and it’s never been a point of conflict with science at all. I see science as a way of uncovering some of the mysteries of God’s creation and in the process having a chance to be even more in awe. Certainly when it comes to this Christmas season, reflecting on the amazing gift that we celebrate, the birth of Christ, that brings that even more into focus. So, yeah I love this opportunity at this time of year, to bring all of those thoughts together.
Doug: Dr. Collins, I consider you a friend, and I hope that we can stay that way.
Francis: I feel the same way, Doug.
Doug: On behalf of the Regenerative Outcomes Foundation, its Board, Advisors, and Research Advisors, I appreciate your willingness to participate in this mission of ours to bring patients access to innovations and the promises of a new age of healing, some of which you’re the architect of. That access is vital to us all, including individuals like myself with a single narrative that has managed to draw wide attention and garner support for these issues. You’re truly a national treasure.
One last question. What is your favorite holiday tradition?
Francis: Before I answer that, let me just say, Doug, thank you. You have emerged as a critical voice at a very important time, and while you say you have a single narrative, you stand in for thousands of narratives, millions of them… others who maybe have not had the chance to be as heard as they need to be. Keep holding us accountable, keep reminding us what really matters. We need to hear from you, as articulately and clearly as you have been doing. Don’t stop.
Doug: Thank you! Now that tradition?
Francis: My favorite holiday tradition is to take my children and grandchildren caroling in the neighborhood with my guitar and an appropriate collection of carols.
Doug: You’ve gone viral, as you know! If I could just be behind you watching that happen! You’re very special. Thank you so much for your time.
The Regenerative Outcomes Foundation www.regenerativeoutcomes.org