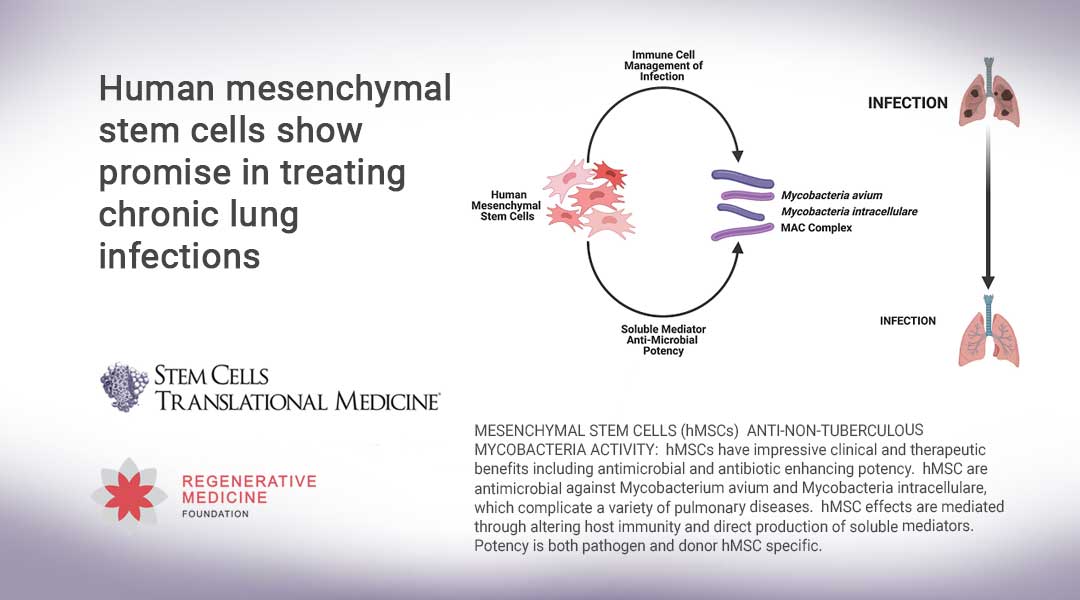
Durham, NC – A study released today in STEM CELLS Translational Medicine offers hope for those suffering from a chronic, difficult to treat condition called non-tuberculous mycobacteria (NTM) lung infection. The study describes how researchers at Case Western University developed a new model of NTM lung infection and then used it to show how effective human mesenchymal stem cells (hMSCs) are in treating this condition – and even which donor cells might be best for doing so.
“The potential to use human mesenchymal stem cells to treat difficult lung infections is promising,” said Anthony Atala, M.D., Editor-in-Chief of STEM CELLS Translational Medicine and Director of the Wake Forest Institute for Regenerative Medicine. “This study shows the ability of using optimal donors to obtain maximum treatment success.”
NTMs are naturally occurring, and everyone inhales them into their lungs as part of daily life. For most people, they are harmless. But in a small number of vulnerable individuals, such as older people or those with cystic fibrosis (CF) or COPD, NTM bacteria can settle in the lungs and cause infection. While not contagious, more than 100,000 people are living with NTM lung disease in the U.S. alone, and that rate appears to be increasing.
“NTM infections can be very difficult to resolve,” said Tracey L. Bonfield, Ph.D., the study’s corresponding author. “Treatment typically requires taking multiple antibiotics, often for years. Patients who suffer from chronic NTM infection not only deal with the consequences of the disease, but also the toxicity, as well as inefficiency and side effects of the antibiotics used to treat it.”
In the search for better therapies, some researchers are focusing on hMSCs, which are collected from adults and can be coaxed into becoming a variety of cells types. hMSCs have significant potential for treating infection and inflammation, Dr. Bonfield said. “They are dynamic storehouses of anti-microbial activity. They are unique in their capacity to respond to infection by secreting multiple bioactive factors, contributing to the host environment. That gives hMSCs a clinical advantage over traditional pharmaceuticals.”
Previous studies by the Bonfield team described the potential for hMSCs and their secreted products (“supernatants”) to treat other types of lung infections including Pseudomonas aeruginosa and Staphylococcus aureus, but these studies are the first to describe the ability of hMSCs to manage two of the most problematic groups of NTMs, Mycobacterium avium (M. avium) and Mycobacterium intracellulare (M. intracellulare). Like these current studies, hMSCs demonstrated significant anti-microbial, anti-inflammatory and anti-fibrotic potential, both in culture medium (in vitro) and in animals (in vivo). Further, they also documented that hMSC treatment improves the effectiveness of antibiotics, leading to a decrease in the dose necessary for eradicating bacteria.
At the same time, those studies pointed out that not all hMSC preparations have the same level of potency or sustainability. “This suggested to us that it is essential to identify the appropriate hMSC donor and subsequent preparation for disease specific applications. That was the goal of our current study,” said Dr. Bonfield.
Both M. avium and M. intracellulare are slow growing bacteria, so researchers have found it difficult to study what happens in sustained NTM infections because in small animals the bacteria clear up quickly, while larger animals are too expensive for defining dosing, timing and duration of a new treatment, Dr. Bonfield noted. So, her team first needed to develop new models of M. avium and M. intracellulare lung infections that would effectively allow them to study this issue.
“In the earlier studies we had developed an innovative protocol in which M. avium and M. intracellulare can be evaluated over the course of a week instead of the typical four to six weeks,” Dr. Bonfield explained. To sustain infection in vivo for chronic disease required an additional innovation “We did this by embedding NTMs into beads of a polysaccharide extracted from seaweed called agarose, and then injecting them into mice with CF. The beads degrade gradually, releasing the NTM into the mice and thus extending the time of infection and inflammatory response. This modeling system has been very efficient in generating acute and chronic scenarios of infection in all of our models.”
The researchers then went on to identify donor-specific hMSC potency against M. avium and M. intracellulare, once again in vitro and in vivo using CF mice. “Every donor hMSC preparation has a unique profile in terms of how the cells respond to pathogens, which likely translates into their successful potency and how the patient responds to hMSC treatment,” Dr. Bonfield said.
“Focusing on hMSC response to NTMs and efficiency of in vitro and in vivo anti-NTM activity provides direction for identifying the optimal hMSC signature for anti-NTM therapy. Data gained from our study begins to define this unique hMSC fingerprint.”
###
The full article, “Donor defined mesenchymal stem cell anti-microbial potency against non-tuberculous mycobacterium,” can be accessed at https://stemcellsjournals.onlinelibrary.wiley.com/doi/abs/10.1002/sctm.20-0521.
About STEM CELLS Translational Medicine: STEM CELLS Translational Medicine (SCTM), co-published by AlphaMed Press and Wiley, is a monthly peer-reviewed publication dedicated to significantly advancing the clinical utilization of stem cell molecular and cellular biology. By bridging stem cell research and clinical trials, SCTM will help move applications of these critical investigations closer to accepted best practices. SCTM is the official journal partner of Regenerative Medicine Foundation.
About AlphaMed Press: Established in 1983, AlphaMed Press with offices in Durham, NC, San Francisco, CA, and Belfast, Northern Ireland, publishes two other internationally renowned peer-reviewed journals: STEM CELLS® (http://www.StemCells.com), celebrating its 39th year, is the world’s first journal devoted to this fast paced field of research. The Oncologist® (http://www.TheOncologist.com), also a monthly peer-reviewed publication, entering its 26th year, is devoted to community and hospital-based oncologists and physicians entrusted with cancer patient care. All three journals are premier periodicals with globally recognized editorial boards dedicated to advancing knowledge and education in their focused disciplines.
About Wiley: Wiley, a global company, helps people and organizations develop the skills and knowledge they need to succeed. Our online scientific, technical, medical and scholarly journals, combined with our digital learning, assessment and certification solutions, help universities, learned societies, businesses, governments and individuals increase the academic and professional impact of their work. For more than 200 years, we have delivered consistent performance to our stakeholders. The company’s website can be accessed at http://www.wiley.com.
About Regenerative Medicine Foundation (RMF): The non-profit Regenerative Medicine Foundation fosters strategic collaborations to accelerate the development of regenerative medicine to improve health and deliver cures. RMF pursues its mission by producing its flagship World Stem Cell Summit, honouring leaders through the Stem Cell and Regenerative Medicine Action Awards, and promoting educational initiatives.