By Angus Chen – Link to Article
In 2010, Doug Olson became the second person in the world to receive CAR-T cell therapy, an experimental tactic to engineer his own immune cells to fight cancer. His doctors had tempered expectations for how well it would fight off Olson’s chronic lymphocytic leukemia, an incurable blood cancer — it was a last stab in the dark, one with no guarantees.
“It was, at the time, an idea way out there,” Carl June, an immunologist at the University of Pennsylvania and the senior researcher on the experiment, said in a call Tuesday with reporters. “In the informed consent document that Doug signed, we thought [the CAR-T cells] would be gone in a month or two.”
But as the researchers tracked Olson and another patient, what they saw was remarkable: Year after year, the CAR-T cells persisted, actively watching for cancer cells. Olson has now been cancer-free for a decade, June and his colleagues reported Wednesday in Nature. The results are so enduring that June dared to use a word that oncologists are usually loath to say: cured.
“We can say it was a cure for Doug, because these are the most mature and oldest results available reported in scientific literature. Because they were the first treated,” June said. “Ten years on, no leukemia cells, and we still have CAR-T cells that are on patrol and surveillance from leukemia.” The first patient treated with CAR-T, Bill Ludwig, also remained cancer-free until his death from Covid-19 in January 2021.
Such enduring results are a landmark scientific achievement for a field that has seen a wave of advances since the first patients were treated a decade ago. There are now approved CAR-T therapies for six different indications including different types of leukemia, lymphoma, and myeloma. Many patients treated with CAR-T therapy so far have eventually experienced a relapse of cancer, making the enduring response from these first two patients extraordinary.
“It’s a big milestone. It makes you think about everything that’s happened in the last 10 years,” said Marcela Maus, an immunologist at Mass General Hospital Cancer Center who was not involved with the work. “These first two patients were both pretty remarkable in terms of long-term remission, and the subjects of a publication that really catalyzed the whole field. It led to the flurry of activity in the biotech space and clinical development of CAR-T as a therapy.”
The new research also provides a close look at how CAR-T cells behave in the body over time, with detailed data from routine blood draws on Olson.
“The new paper really describes in great detail what happened to the first two patients,” Maus said. “As an immunologist, it’s really interesting to see the evolution of a very specific T cell response, when you know exactly the day they went in and had an exposure, then carefully followed over 10 years.”
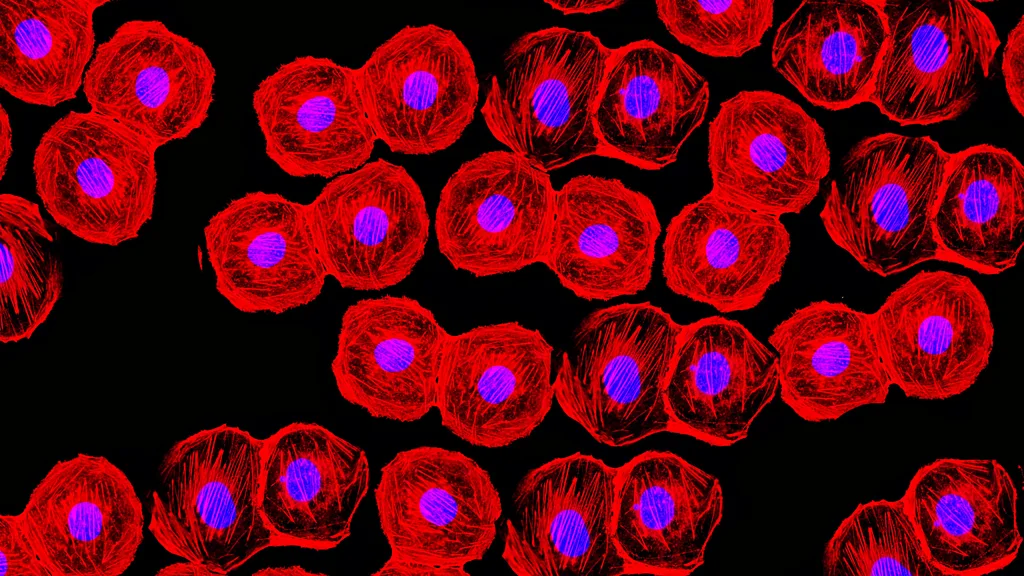
The therapy works by isolating immune cells known as T cells from the patient’s body. Then, researchers use a virus to genetically engineer a synthetic receptor — known as a CAR, or chimeric antigen receptor — onto the T cell’s surface. This CAR can bind to a specific target, in this case a protein found on immune B cells called CD19, and it can activate the T cell to kill any cell bearing this target. Because chronic lymphocytic leukemia, the cancer that Olson and Ludwig had, are malignancies of the B cell, the engineered cells could recognize cancerous B cells and destroy them.
Olson didn’t notice any changes in the weeks after he received his first infusion in December 2010. Then he started to feel seriously ill — as if he’d been floored by a terrible flu – and he was hospitalized. At this time, the data suggest that the CAR-T cells he’d just received were proliferating rapidly as a type of T cell known as a killer T-cell. These are known as CD8 cells, and they were assassinating every cancer cell they could find.
“You kill large numbers of cancer cells, and they spill their contents into the blood. That can make people quite sick and cause damage to kidneys which Doug did have,” explained David Porter, Olson’s oncologist at the University of Pennsylvania.
Olson also experienced some symptoms often attributed to cytokine release syndrome, which happens when CAR-T cells flood the body with cytokines, immune compounds that white blood cells use to kill. It can cause flu-like symptoms in some patients, but in some cases, these cytokine storms can lead to fluid leaking into the lungs, extreme fevers, neurological damage, and even death.
At the end of Olson’s three-day stay in the hospital, Porter told him that about 18% of his white blood cells were CAR-T cells. The next week, Olson went back for a check-up. Both he and Porter were delighted and shocked by the result.
“Doug, we cannot find a single cancer cell in your body. Your bone marrow is completely free of [the cancer],” Porter told him. It took roughly another six months after treatment for certain markers of residual disease to go away.
Over the next several months, the data suggested that the patients’ CAR-T cells were transforming from the killer CD8 T cells and into CD4 T cells, or “helper” T cells. These tend to remain in the body and help form a long-term immune memory, but typically are less involved in actively killing diseased cells.
In the years that followed, the CAR-T cell population did what our own natural T cells normally do: shift back and forth between types. By the nine-year mark, the researchers could only find CD4 cells, suggesting that the cells had stabilized into a long-term population of helper T cells.
When the scientists isolated those CD4 cells nine years after treatment, they bore markers that usually suggest immune cells are too exhausted to keep doing their work. Despite that, these CD4 CAR-T cells could still recognize and unexpectedly destroy cancer cells in the lab, which led June and his colleagues to suspect that the cells were preventing the return of cancer in the patients by killing off any B cells the body makes.
Immunologists are now speculating about what these observations might mean about the evolution of CAR-T cells in the body and why they work so spectacularly for some patients. Maybe there’s something special about a CAR in a CD4 cell that makes the T cells still functional after so many years. Maybe having a flexible population of CAR-T cells that can shift between different types — including CD4, CD8, and gamma-delta T cells — is important, MGH’s Maus mused. “Multiple cells can have effects, and maybe more than one is better,” she said.
It’s exactly the kind of brainstorming the authors wanted to spark — questions whose answers could ultimately help scientists “generate the next iteration of therapies,” said Joseph Melenhorst, an immunologist at the University of Pennsylvania and the lead author of the paper.
For Olson, the results point to a reason for optimism, at least for some patients, when options are scarce. “That day back in 2010 when I was infused with my CAR-Ts, and my tumor cells disappeared – it meant there was a whole new treatment paradigm,” he said. “ [For cancer patients], it’d make a big difference in their hope. And if there’s no cure for [them] today, there’s a possibility that around the corner, there will be.”