Article from Helio.com – Link to article
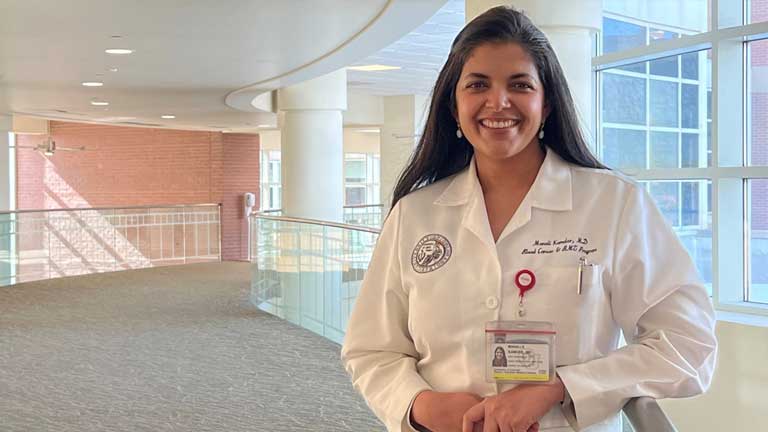
Results from a randomized phase 3 study saw one CAR-T significantly outperform the current standard of care among patients with relapsed or refractory disease, according to study investigator Manali Kamdar, MD. “The patients I have treated with [CAR-T] ended up having a better quality of life,” she said. Source: Erin Carlson, RN/University of Colorado .
Since the approval of the first chimeric antigen receptor T-cell therapy, the research community has grappled with a crucial question.
Is the modality appropriate for earlier use by patients with certain types of cancer?
Despite positive signals from clinical trials, the typical answer had been a cautiously optimistic “maybe.”
Data presented in December at ASH Annual Meeting and Exposition has shifted the consensus more toward the affirmative.
The randomized studies — which compared commercially available CD19-directed CAR-T with standard therapy for patients with advanced B-cell non-Hodgkin lymphoma — yielded a split decision about which of the three approved CAR-T products should be considered as second-line therapy.
Axicabtagene ciloleucel (Yescarta; Kite Pharma/Gilead Sciences) and lisocabtagene maraleucel (Breyanzi, Bristol Myers Squibb) conferred statistically significant improvements in EFS compared with hematopoietic stem cell transplantation, the current standard for patients who are resistant to chemotherapy or whose disease relapses within 12 months of front-line treatment.
A third CAR-T — tisagenlecleucel (Kymriah, Novartis) — did not significantly extend EFS compared with HSCT.
It has been about 2 decades since such effective new therapeutics have been developed for this high-risk population, according to Manali Kamdar, MD, associate professor of medicine/hematology at University of Colorado School of Medicine and clinical director of lymphoma services at CU Cancer Center.
“The results speak for themselves,” Kamdar, who presented results of the lisocabtagene maraleucel trial at ASH, told Healio. “[The findings] have the potential to cause a paradigm shift in the standard of care.”
Healio spoke with researchers from each of the three pivotal trials, as well as other lymphoma specialists, about the results and the impact they will have on treatment of relapsed or refractory B-cell NHL.
TRANSFORM, ZUMA-7 show improved efficacy, safety
The multicenter TRANSFORM trial compared lisocabtagene maraleucel, often called liso-cel, with standard therapy — which included salvage therapy followed by high-dose chemotherapy and HSCT — for adults with previously treated diffuse large B-cell lymphoma.
At an interim prespecified analysis with a median follow-up of 6.2 months (range, 0.9-20), the study achieved its primary endpoint of improved median EFS with liso-cel (10.1 months vs. 2.3 months; HR = 0.34; P < .0001). Liso-cel also significantly extended median PFS (14.8 months vs. 5.7 months; HR = 0.4; P = .0001).
Researchers reported no cases of grade 4 or grade 5 cytokine release syndrome or neurotoxicity. One patient developed grade 3 CRS and four (4%) had grade 3 neurotoxicity.
Approximately one-third of patients like those treated in the TRANSFORM trial typically would respond to standard second-line therapy and only one-quarter would achieve long-term remissions, Kamdar said.
“This trial not only showed that lisocabtagene maraleucel is more efficacious but is also absolutely manageable with respect to its safety profile,” Kamdar said. “Given that this high-risk patient population doesn’t have favorable outcomes, it would be a positive development to have the liso-cel label expanded to second-line therapy.”
The randomized, multicenter ZUMA-7 trial yielded similarly positive results.
Researchers compared axicabtagene ciloleucel — often called axi-cel — with standard chemotherapy plus HSCT for patients with relapsed or refractory DLBCL.
After median follow-up of 24.9 months, the trial met its primary endpoint by demonstrating a fourfold increase in median EFS with axi-cel (8.3 months vs. 2 months; HR = 0.39; 95% CI, 0.3-0.51). Researchers also reported a higher overall response rate (83% vs. 50%; OR = 5.31; 95% CI, 3.1-8.9) and complete response rate (65% vs. 32%) in the axi-cel group.
Six percent of patients assigned axi-cel developed grade 3 or greater CRS, and 21% had grade 3 or greater neurotoxicity. No cases of grade 5 CRS or neurotoxicity occurred.
“This is the biggest breakthrough we have seen for patients with diffuse large B-cell lymphoma who are resistant to chemotherapy,” trial investigator Lori A. Leslie, MD, assistant professor at Hackensack Meridian School of Medicine and director of the indolent lymphoma and chronic lymphocytic leukemia research programs at John Theurer Cancer Center, told Healio.
Leslie said she is “extremely excited” that more patients may be eligible to receive axi-cel earlier in their disease course if the FDA expands the agent’s label.

Lori A. Leslie, MD
“This shows that CAR-T is giving a long-term benefit with a one-and-done approach while avoiding the toxicities of salvage chemotherapy and autologous transplant for patients with high-risk disease,” Leslie said. “If there is an approval, then it would immediately change the standard of care for high-risk patients who are either primary refractory or have early relapse after front-line therapy.”
Investigators ‘shocked’ by BELINDA results
Tisagenlecleucel is considered the dean of CAR T-cell therapies, given its distinction of being the first approved for commercial use in the United States.
However, a final analysis of the BELINDA trial — presented during ASH’s late-breaking abstract session — showed the therapy failed to significantly improve outcomes compared with standard therapy for advanced B-cell NHL.
The multicenter study included patients with primary refractory aggressive B-cell NHL or those whose disease relapsed within 12 months of first-line treatment. Researchers randomly assigned patients to tisagenlecleucel or salvage chemotherapy and autologous HSCT. EFS served as the primary end
After median follow-up of 10 months (range, 2.9-23.2), results showed median EFS of 3 months for both the tisagenlecleucel and standard groups (adjusted HR = 0.95).
An analysis of best overall response 12 weeks or more after therapy showed ORRs of 46.3% in the tisagenlecleucel group and 42.5% in the standard group.
“We were shocked by the results,” Michael R. Bishop, MD, director of The David and Etta Jonas Center for Cellular Therapy at The University of Chicago and BELINDA trial steering committee chair, told Healio.
Issues with the trial design — including study endpoint definitions, the use of prior bridging therapies and time to infusion — influenced the results, Bishop said.
“We can learn from this trial, and this is the reason we do phase 3 studies,” Bishop added. “We believe that if tisagenlecleucel had been used differently, then there would have been benefit derived from it.”
Despite the results, Bishop noted tisagenlecleucel remains beneficial for 40% of patients with advanced large B-cell lymphoma based on long-term data from the JULIET trial, in addition to its known efficacy for pediatric ALL.
“Unfortunately, when it comes to the way we provided the treatment in BELINDA trial, I cannot say that tisagenlecleucel [provides] benefit for the subset of patients with early relapse or primary refractory diffuse large B-cell lymphoma.”
The reasons for tisagenlecleucel’s inability to produce a significant increase in EFS in the BELINDA trial are unclear, according to Joshua Sasine, MD, PhD, assistant professor of medicine and director of the CAR T program at Cedars-Sinai Cancer.
Why did tisagenlecleucel fail where axi-cel and liso-cel succeeded?
“Perhaps not all CAR-T products are created equal,” Sasine told Healio.

Joshua Sasine, MD, PhD
“One explanation could be the complexity of the [BELINDA] trial design, which might have diluted a benefit that could have otherwise been seen,” he added. “Of course, the other explanation could be that [tisagenlecleucel] is not better than standard-of-care therapy.”
Catherine S. Diefenbach, MD, associate professor of medicine, clinical director of lymphoma and translational director of hematology at NYU Langone’s Perlmutter Cancer Center, also cited issues with the BELINDA trial design. The CAR design itself also could have contributed to tisagenlecleucel’s lackluster performance compared with the outcomes observed in the ZUMA-7 and TRANSFORM studies, she added.
“Each trial was designed slightly differently with respect to patient populations and bridging therapy,” Diefenbach told Healio. “Time will tell where Kymriah finds its place but, as things currently stand, its label will not be expanded to second-line treatment.”
Patient selection also could explain why tisagenlecleucel failed to demonstrate superiority vs. standard therapy, according to Joseph M. Tuscano, MD, professor of medicine in the division of hematology and oncology at UC Davis Comprehensive Cancer Center and panel member of the National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology for B-Cell Lymphomas.
“Patients with more aggressive lymphoma may have been enrolled in the BELINDA trial given that bridging therapy was not allowed in the TRANSFORM and ZUMA-7 studies but was permitted in the BELINDA study,” he told Healio.
Longer follow-up is needed in the BELINDA and TRANSFORM studies, he added, as only the ZUMA-7 trial had median follow up of more than 2 years.
Looking for ‘a big win’
The decision about whether to expand the use of CAR-T to a larger number of patients is swiftly approaching.
Kite Pharma submitted a supplemental biologics license application to the FDA in October 2021 seeking to expand the axi-cel label to include second-line therapy for adults with relapsed or refractory large B-cell lymphoma. The FDA accepted the application and granted it priority review designation, establishing a target action date of April 1.
Data presented at ASH regarding safety, efficacy and patient-reported outcomes all point toward axi-cel being a more effective and tolerable treatment than the decades-old standard approach, according to a statement Kite Pharma provided to Healio.
“There are moments in oncology history and ZUMA‐7 is one of them,” the statement read. “With these superior clinical outcomes, coupled with an improved quality of life for these patients, we believe Yescarta has the potential to shift the way in which patients with [large B-cell lymphoma] in the second‐line setting should be treated and should be considered the new standard of care, if approved.”
Bristol Myers Squibb does not comment on regulatory submission timelines, but a spokesperson indicated the company plans to approach the FDA to expand the label for liso-cel at some point.
“Data from TRANSFORM are potentially practice‐changing,” the company said in a statement to Healio. “We are completing a full evaluation of the TRANSFORM data, and we look forward to sharing with regulatory authorities for review with the goal of bringing Breyanzi to more patients in need.”
Based on convincing data from the TRANSFORM and ZUMA-7 studies, lymphoma specialists with whom Healio spoke agreed the FDA ultimately will expand the labels for axi-cel and liso-cel to include second-line therapy for B-cell NHL. The key question remains which patients would qualify, allowing them to undergo CAR T-cell therapy without prior autologous HSCT.