Remarkable achievement in volumetric bioprinting opens new opportunities for regenerative medicine and drug development
By Davide Sher – 3D Printing Network – Link to article
A team from Utrecht University (Netherlands), working on novel 3D bioprinting technologies and on their application in medicine and biomedical research, just published a new study on volumetric bioprinting of large-scale, functional liver units. The study, titled “Volumetric Bioprinting of Organoids and Optically Tuned Hydrogels to Build Liver-Like Metabolic Biofactories”, was published in the journal Advanced Materials (Wiley), one of the leading scientific journals in materials science and 3D printing. It is open access, currently e-published ahead of print, with more figures and content available in the supplementary information.
As Riccardo Levato, Associate Professor from Utrecht University and one of the study’s authors, told 3dpbm, the researchers were able to ultra-fast (<20 seconds) volumetric bioprinting of large scale (>1 cm3) engineered liver units, that are functional and able to perform key toxin elimination processes that natural livers perform in our body. To achieve this breakthrough, they developed a new method to perform Volumetric Bioprinting by means of visible light tomography. The ability to bioprint such large functional units of the liver will open new opportunities for regenerative medicine and drug development testing (DDT).
Previously, in 2019, 3dpbm covered the story of the achievement by the same team when they first pioneered this layerless technology in the realm of biofabrication. It should be noted that volumetric bioprinting, a type of 3D printing that enables the construction of parts and constructs from all sides at the same time, is considered key to achieving 3D bioprinting of complex organs in the future. From that work, a spin-off from the team’s collaborators in Lausanne, Readily3D (who is also involved in this new study) came into being.
Seeing through cells
 The research team developed a technique to “make cells transparent”, so that they could overcome one of the main limitations of volumetric printing, which is to avoid printing artifacts and the loss of resolution due to light scattering caused by cells. In this way, volumetric bioprinting becomes truly accessible to all cell printing applications. As volumetric printing relies on the precise patterning of light in 3D, it is typically only possible in highly transparent materials. However, cells at high concentrations can scatter light, to the point of impeding certain prints.
The research team developed a technique to “make cells transparent”, so that they could overcome one of the main limitations of volumetric printing, which is to avoid printing artifacts and the loss of resolution due to light scattering caused by cells. In this way, volumetric bioprinting becomes truly accessible to all cell printing applications. As volumetric printing relies on the precise patterning of light in 3D, it is typically only possible in highly transparent materials. However, cells at high concentrations can scatter light, to the point of impeding certain prints.
In this work, the researchers developed a new material formulation using a bio-friendly compound, used nowadays in medicine as a contrast agent for coronary angiography (iodixanol) which can essentially “make the cells transparent”. In this way, they can allow high printing fidelity even at high cell density, which is needed for tissue engineering applications. Moreover, similar strategies could be used outside the realm of bioprinting, for instance, to print composite resins with micro and nanoparticles (ceramics, metals, etc.).
The researchers were able to build a large (>1 cm3) viable and functional liver unit, for the first time by printing organoids. Organoids are miniaturized (max 1 mm), stem-cell made units that copy some aspects of their tissue of reference. Alone, they cannot be easily assembled into large structures, needed to mimic human organs, limiting their capacity to be used in clinical settings. The use of safe light, ultra-rapid fabrication rate and the contactless nature of volumetric bioprinting (so that there is no shear stress on the cells) permit to keep the organoids safe and alive.

Overview of the high-resolution volumetric printing process and study design. A) Schematic representation of the volumetric printing process. B-C) Highest resolution prints of B) positive and C) fully perfusable negative features achieved with the 5% gelMA+ 0.1% LAP bioresin used in this study (scale bars = 1 mm). Samples were imaged when being immersed in PBS directly after printing.D) Diagram of the hepatic organoid culture system, starting with human liver biopsies and isolation into single cells, which are then dynamically cultured in a spinner flask system to establish high yields of hollow epithelial organoid structures (microscopy image scale bar = 250 μm). E) Illustration of a complex, organoid-laden printed biofactory cultured under dynamic perfusion to This article isprotected by copyright. All rights reserved.41enhance hepatic function, showing a representation of the breakdown of perfused compounds (purple circles) into metabolites (black squares). Figure 2: Effect of single-cell and organoid density on volumetric bioprinting accuracy in absence of optical corrections. Fine feature thickness in constructs printed at increasing light doses (250 –625 mJ cm-2) with bioresins containing different densities of (A) single cell and (B) organoid (1 –5 x 106cells mL-1). The dashed line represents the programmed feature dimension of the printed model (selected to be 500 μmto accommodate for the size of the printed organoids)(n = 3).
Biological function follows (printed) form
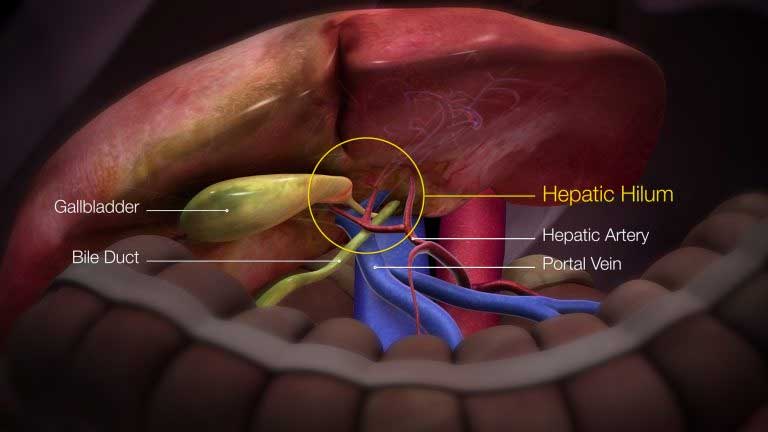
The Utrecht University research team demonstrated how printing cells into different 3D architectures can boost their ability to work as a liver, an indication that bioprinting can really be used to improve the functional resemblance between printed structures and native tissues. They also demonstrated this showing how the printed architecture successfully improved the ability of the organoids to detoxify and eliminate compounds that could be harmful for our body. “Via bioprinting, we also create different porous structures that can be perfused with nutrients, and “replace” the role of blood vessels,” Riccardo Levato told 3dpbm. “These bioprinted liver units of such clinically relevant sizes open new opportunities for regenerative medicine and for developing new patient-specific models to study new drugs against liver diseases.”