By Stem Cells Translational Medicine –
Abstract
In biliary atresia (BA), it has been demonstrated that biliary epithelial-mesenchymal transition (EMT) of reactive ductular cells is associated with liver fibrosis. This study aimed to develop an ex vivo biliary EMT model of liver ductal organoids for exploring the involvement of biliary EMT in fibrogenesis and to investigate whether human amniotic fluid stem cells (hAFSCs) can mitigate the biliary EMT process.
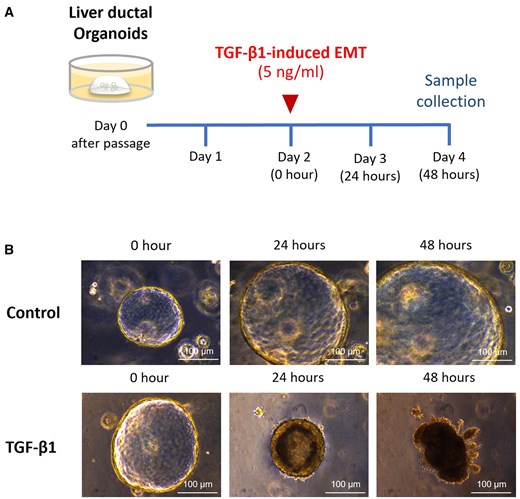
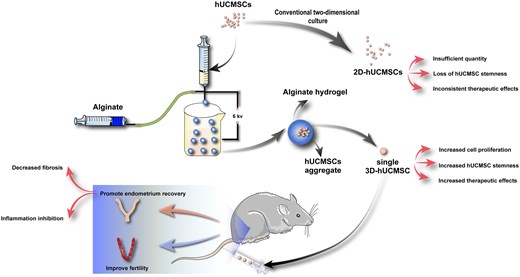
Liver ductal organoids were generated from the intrahepatic bile duct of healthy neonatal mice. Biliary EMT was induced in organoids by the administration of transforming growth factor beta-1 (TGF-β1) in culture medium. hAFSCs were co-cultured with organoids during biliary EMT induction. Expression of biliary epithelial cells, mesenchymal cells, myofibroblast, collagen I, and genes related to the Wnt signaling pathway were evaluated.
Following administration of TGF-β1, we observed an increased expression of mesenchymal cell markers N-cadherin and Vimentin, as well as myofibroblast marker alpha-smooth muscle actin (α-SMA) in liver ductal organoids which were associated with increased expression of collagen 1. Administration of hAFSCs to organoids significantly attenuated TGF-β1-induced biliary EMT and collagen production. In addition, Wnt signaling was upregulated in biliary EMT, while hAFSCs downregulated the Wnt signaling resulting in decreased expression of myofibroblast and collagen in organoids.
TGF-β1 is a potent cytokine that induces biliary EMT. hAFSCs significantly mitigated TGF-β1-induced biliary EMT in liver ductal organoids. The beneficial effect of hAFSCs administration is associated with the downregulation of the Wnt signaling pathway. This study indicates that hAFSCs can prevent the progression of liver fibrosis in BA.